Key points
• Axillary surgery is performed either during breast cancer surgery or separately to assess if there is lymph node involvement and to what extent.
• Axillary surgery includes: sentinel lymph node biopsy, axillary node sampling and axillary lymph node dissection.
• Removal of lymph nodes helps to determine if further treatment is required based on the number and type of cancer cells detected in the lymph nodes.
• The risk of lymphoedema is low post sentinel lymph node biopsy; this risk increases post axillary node dissection.
Axillary Surgery
Axillary surgery is routinely performed during breast conserving surgery for invasive breast cancer or when a mastectomy is the surgical option to examine for any lymph node involvement of cancer cells. This information is used to assess breast cancer stage and to help determine the recommended treatment plan and individual prognosis. The removal of known positive lymph nodes helps to minimise both local recurrence and distant metastases.
Three types of axillary surgery
Sentinel lymph node biopsy (SLNB)
This procedure is performed when there is no evidence of spread to the lymph nodes at initial imaging and cancer diagnosis.
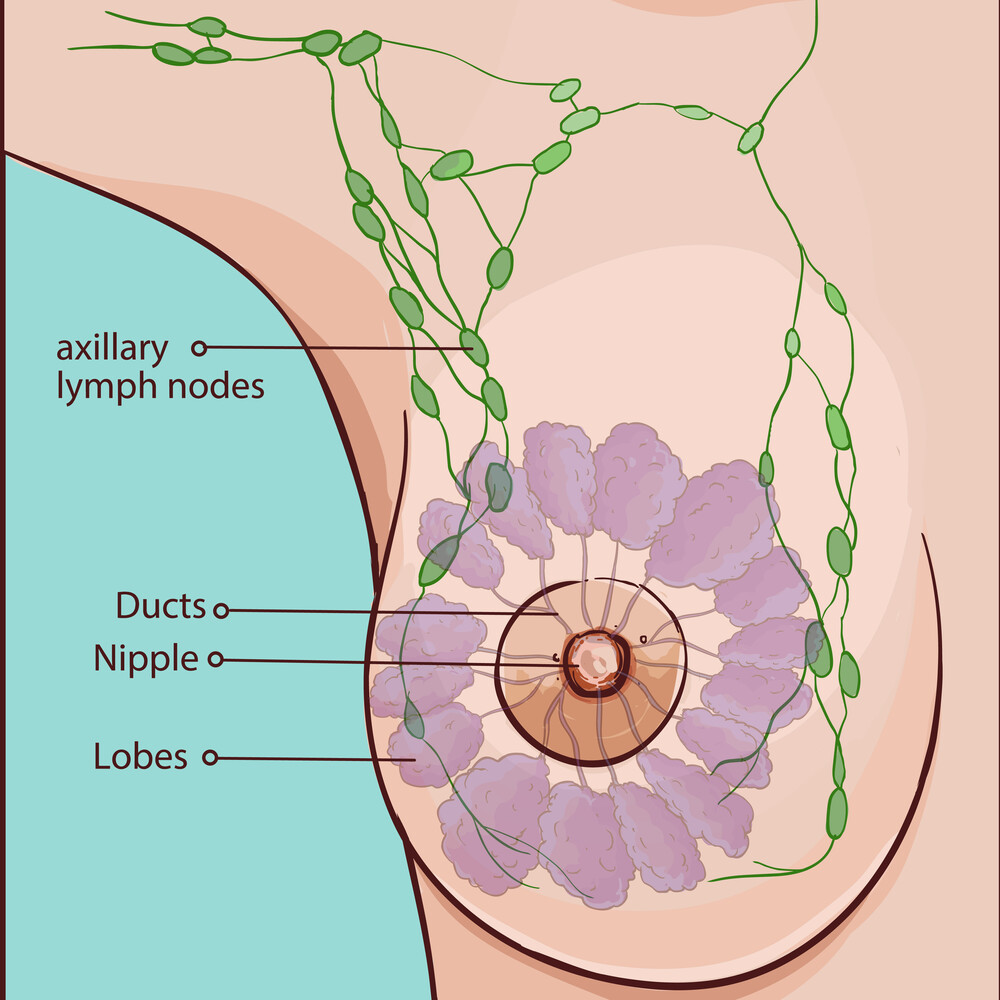
The sentinel node(s) is the first draining lymph node(s) in the underarm that drains lymphatic fluid from the breast. The node is identified by injecting a dye or radioactive isotope around the areola or primary tumour. The dye and/or radioactive isotope will reach the sentinel node first, which is identified by the surgeon using either a gamma probe or visually noting the blue staining from the dye. Once identified this is then surgically removed, and sent to pathology to investigate for the presence of cancer cells.
If no cancer cells, or only isolated cancer cells, are found in the sentinel node, no further nodes are removed. If cancer cells are present, an axillary dissection or radiation therapy to the axilla may be recommended. If micrometastases (deposits measuring less than 2mm) are identified, the patient may not need further axillary dissection, as when appropriate adjuvant treatment is given the risk of recurrence in the axilla is low.
The surgeon may opt to perform an intraoperative frozen section of the sentinel lymph node to gain an immediate answer for the presence of cancer cells so can proceed to an axillary lymph node dissection during the same theatre time if this result is positive and to avoid a second surgery.
The blue dye injected into the breast to locate the sentinel node may leave some staining on the skin around the injection site, but will fade over a few weeks. The risk of developing lymphoedema (chronic swelling of the affected arm) is low with SLNB.
Axillary node sampling
Axillary sampling is when at least four lymph nodes are removed (usually from the lower axilla) to improve detection rate or help stage the axilla by testing for cancer cells. If detected, an axillary lymph node dissection may be recommended. If axillary lymph node dissection is not performed, radiation therapy should form part of the patient’s treatment plan to reduce the risk of axillary recurrence.
Axillary node dissection
Lymph nodes are removed in levels one (lower) and two (mid) of the axilla, which can involve removing between 5–30 nodes. Nodes in level three (high) are not routinely removed, unless there is known disease, due to an increased risk of complications, including lymphoedema, nerve damage and parathesia, and shoulder injury, without improving patient outcome.