Benign conditions presenting as lumps
Benign conditions, such as mastalgia, mastitis, breast cysts and fibroadenomas, can present as clinical symptoms of breast cancer.
Fibrocystic change:
Fibrocystic change is the most common cause of breast lumps in women aged 30-50. It is a result of breast tissue overreacting to normal hormone changes in the menstrual cycle. This can cause scarring around the ducts, causing tiny cysts to develop. Fibrocystic lumps feel smooth and mobile, may fluctuate in size during the menstrual cycle, and breast tenderness is common. Spontaneous green or brown nipple discharge may also be present. Fibrocystic lumps usually require no treatment, however larger cysts causing more severe pain may require aspiration. Fibrocystic breast changes do not increase the risk of developing breast cancer.
Sebaceous cyst:
These cysts develop in sebaceous glands, and are commonly seen on the face, back and neck and in the breast skin. They are visible on mammograms as well-circumscribed rounded soft tissue lesions close to the skin surface. Sebaceous cysts are usually surgically removed as they tend to reoccur and become infected. They can also be removed for cosmetic reasons.
Hamartoma:
Hamartomas result from an overgrowth of fibro-glandular and fatty tissue within a thin capsule of connective tissue. It usually presents as a painless soft lump, but can sometimes lead to a unilateral breast enlargement without a palpable localised lump. It is usually detected by mammogram but requires a biopsy to confirm the diagnosis. They are typically treated with surgical removal.
Lipoma:
Lipomas are benign fatty lumps or tumours that occur anywhere in the body where fat cells are found. They are painless, mobile lumps that are mostly asymptomatic, and in the vast majority of cases are incidentally found during routine breast screening. No treatment is required unless they are producing symptoms or show signs of growing.
Fibroadenomas:
Fibroadenomas usually present as a lump or a change detected on ultrasound/mammogram. Fibroadenomas can vary in size, with some women having more than one. Diagnosis is by core biopsy.
Fibroadenomas are common and thought to be related to estrogen. Although they can appear at any age, they are more likely when aged 15-40 years.
Fibromas are found in the breast lobule and fibrous tissue. Fibroadenomas occurs when tissue in the lobule overgrows and becomes hard.
Most will shrink over time, so are usually left alone. If a fibroadenoma becomes larger or is painful referral to a breast specialist should be made regarding excision.
Mastalgia
Cyclical pain: Cyclical breast pain is related to normal hormonal changes in the menstrual cycle. Breast tenderness can develop in the second half of the menstrual cycle, worsening in the days before a woman’s period. Cyclical breast pain typically occurs in both breasts, particularly in the upper outer region, as this has the greatest concentration of glandular breast tissue. Women may notice their breasts feel more ‘lumpy’ than usual during this time. If the pain is mild, and no other concerning symptoms are evident, no further treatment will be required. Pain alone is generally not a sign of breast cancer.
Non-cyclical pain: Non-cyclical breast pain has no relation to the menstrual cycle and is more likely to affect women aged over 40. Pain or tenderness can be constant or intermittent, and may be felt in one or both breasts. There may be no obvious cause or underlying abnormality for this pain, or it may be due to the following:
- Referred pain from the neck or chest wall. This can be due to trauma, muscle strain after repeated upper body activity or chest infection.
- Pregnancy or breast-feeding.
- Large breasts, which can cause supportive ligaments to stretch, resulting in pain.
- Costochondritis (Tietze's Syndrome): The inflammation of cartilage in the rib cage, usually where the upper ribs attach to the sternum. It usually resolves without treatment after four to six weeks and seldom returns.
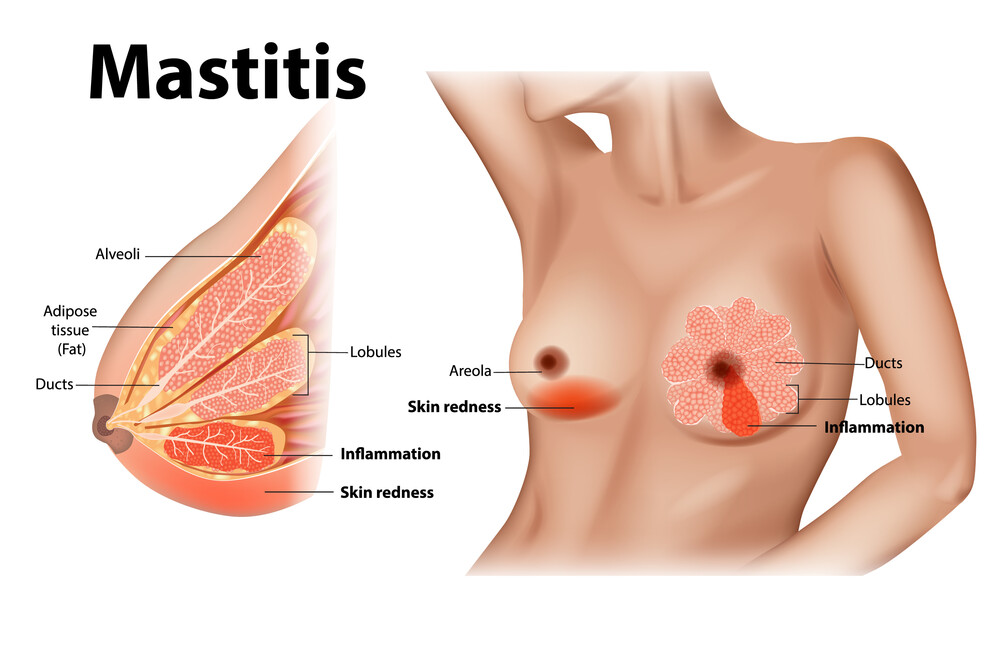
Mastitis: Mastitis is the inflammation of breast tissue. This can be caused by milk trapped in the breast or a blocked milk duct (if breast-feeding) or an infection. Mastitis is usually resolved with antibiotics. Periductal mastitis can occur when the ducts under the nipple become infected. This condition often recurs as the damaged ducts remain, even after treatment, and in severe cases the ducts may need to be removed.
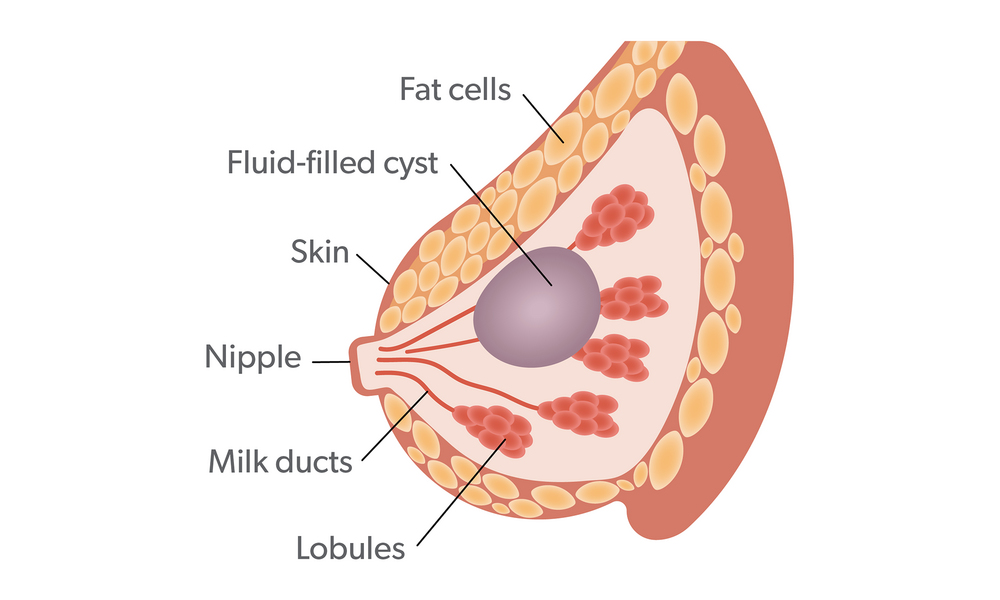
Breast cysts: Breast cysts may occur naturally with ageing, due to a fall in oestrogen levels. They are most common over the age of 35 but occurrence drops after menopause. Women on hormone replacement therapy may still develop cysts. Cysts can vary in size – they may be too small to be palpable or may present as a lump – and so cannot be reliably diagnosed by clinical examination alone. Simple cysts require no treatment, but if causing discomfort, refer to a breast clinic for drainage. Ultrasound should be performed before this procedure to confirm whether it is solid or cystic. A needle biopsy may be necessary to exclude breast cancer.
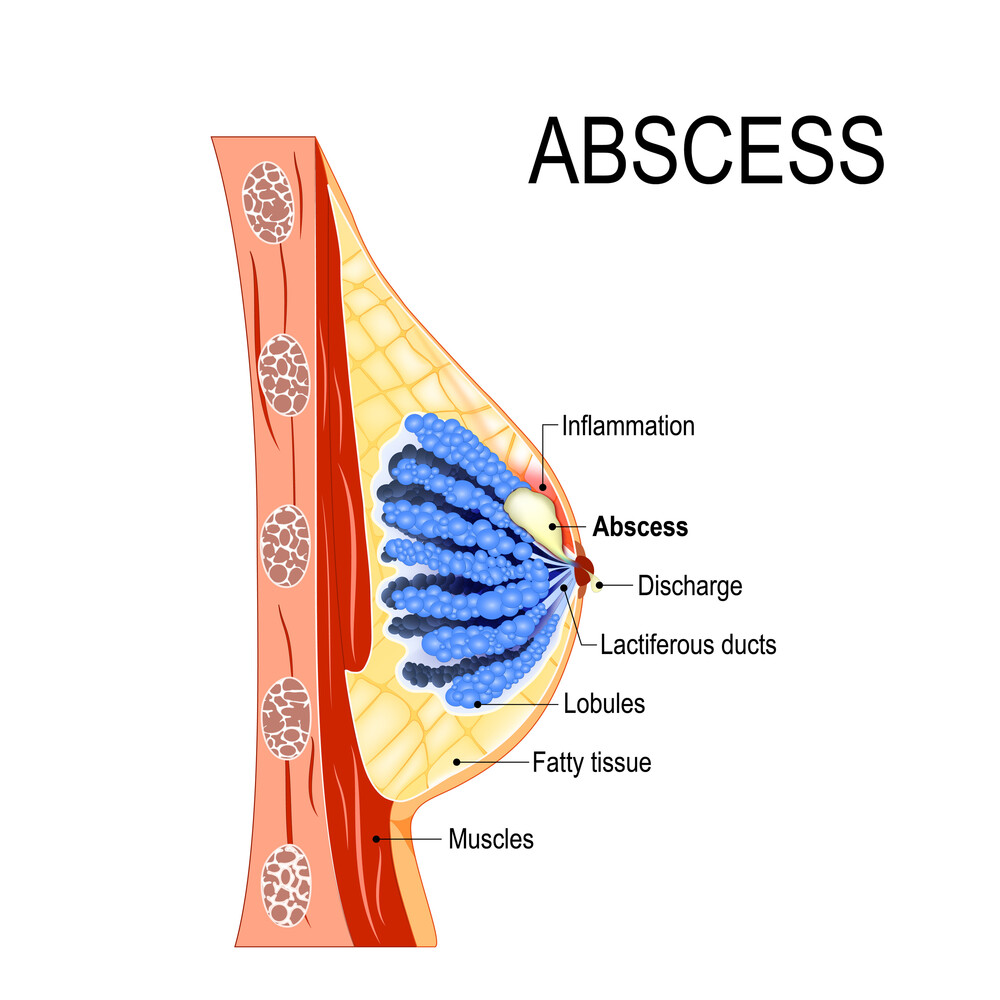
Breast abscess: Abscess may follow an occurrence of mastitis, requiring excision and drainage. Mastitis or breast abscess in a non-lactating woman requires further investigation for an underlying condition or malignancy.
Abscess picture
Physical changes
Nipple discharge: Benign nipple discharge is not spontaneous, and it tends to be bilateral, expressed from multiple ducts. Up to 20% of women are able to express fluid from their nipples. Discharge is commonly creamy, brown or green. Galactorrhoea (milky discharge) is usually caused by an overproduction of prolactin due to certain medications, excessive breast stimulation or pituitary gland disorders. Conditions such as intraductal papilloma, duct ectasia and fibrocystic change can also produce nipple discharge. Any discharge that occurs without squeezing, comes from a single duct in the nipple and is clear or blood-stained should be investigated to exclude breast cancer.
Nipple/areola eczema: Eczema in this area usually starts on the areola and can spread to the nipple. It usually resolves when treated with topical corticosteroid creams. If the ‘eczema’ on the nipple persists or worsens, patients should be referred to a breast clinic to exclude Paget’s Disease of the breast.
Accessory nipples or breast tissue: This condition, which can occur in men and women, is a result of leftover foetal breast tissue and is present from birth. Accessory nipples usually occur on the lower part of the breast but can be found anywhere along the embryonic milk lines. Treatment involves surgery for cosmetic reasons or due to ulceration or other clinical concerns.
Accessory breast tissue is a prominent swelling containing extra breast tissue. It is mostly found in the axilla but more than one site may be involved. Both benign and cancerous breast conditions can occur in this tissue. Most cases of accessory breast tissue are so small as to go unnoticed, but large problematic, areas can be treated with surgery and/or liposuction of the tissue.



